When Javeria and Usman Ahmad’s newborn son Ismaeel was diagnosed with a rare genetic immunodeficiency disorder, they rushed to proceed with a bone marrow transplant from Usman, even though, as a parent, he was only a “half match”, bringing added risks.
Their first son, Zakariya, had died at just 15 months of the same condition – severe combined immunodeficiency (SCID).

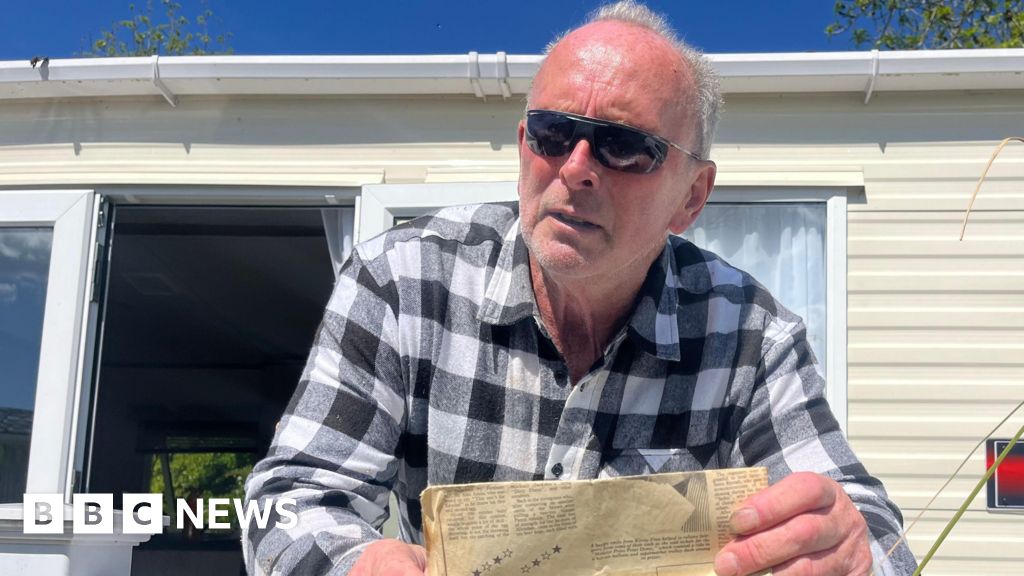
Javeria Ahmad, with her son Ismaeel, now 10, who needed a bone marrow transplant as a baby. Credit: Steven Siewert
“They spent six weeks looking in the donor registries around the world, and we couldn’t find anything better than a 30 per cent match,” Javeria said. She was preparing to donate when Zakariya’s condition deteriorated.
A shortage of bone marrow donors is causing problems for Australians, particularly those from diverse backgrounds. Like many, the only option for the Ahmad family, who have Pakistani heritage, was a partial match from a relative.
Donation advocates hope the now-widespread availability of cheek swab testing will encourage more young people from all ethnic backgrounds to become donors. Registering, previously only available via a blood draw, is now as simple as returning the cotton swab sample by mail, resulting in a potential match for a current or future patient.
Usman donated through a process similar to giving blood. He returned to work the next day, while Javeria sat with Ismaeel as the stem cells were administered via his chest.
“I was just holding him on my lap as the cells went in,” she said. “The procedure itself was quite uneventful.”
It was also a success. Ismaeel is now an active 10-year-old who loves soccer and basketball, and regularly tops his class. He will probably receive fortnightly antibody infusions from donated blood plasma for the rest of his life, but his parents, from Sydney’s west, hope he won’t need another transplant, though there’s always the chance.
Loading
Dr Sam Milliken, the head of haemotology at St Vincent’s Hospital in Sydney, said half-match or “haploidentical” transplants have a slightly lower chance of success, as well as a higher risk of graft-versus-host disease, where the new immune system in the donated cells attacks the patient.
“These days it’s not such a big problem,” he said. “We’re able to control [graft-versus-host] ... because of new techniques.”
Lisa Smith, chief executive of Stem Cell Donors, which manages the national registry, said treatment protocol was still to find “as good a match as possible”.
Australia’s donor pool of 175,000 is too small to support the 2000 people needing a transplant each year. About 40 per cent of patients have diverse ancestry. Those with North African and Middle Eastern backgrounds are least likely to find a match, followed by patients with South-East Asian ancestry.
Loading
Only about 100,000 donors are aged 18 to 35, considered the most successful age. While donors stay on the registry until age 60, new over-35s cannot join and most patients – 80 per cent – receive a donation from overseas.
“We just don’t recruit enough donors in Australia … there’s just been a lack of investment,” Smith said.
In March 2024, the federal government allocated $2 million to increase donations, including through cheek swab testing, following $1 million in 2023.
Smith said Stem Cell Donors now recruited about 15,000 donors a year, up from 5000 a few years ago, but 25,000 to 40,000 would be ideal, and the funding is not ongoing.
A spokesperson for the Department of Health said it remained committed to “ongoing, collaborative efforts” to ensure the size and quality of the registry, pointing to a 6 per cent increase in donors with self-reported diverse ancestry since 2023.
Pamela Bousejean, founder of UR the Cure, hopes cheek swabs will help Australia catch up with countries, including the US, which adopted them in the early 2000s.
Bousejean, who was diagnosed with Hodgkin lymphoma in 2010, was told her “only chance” of survival was a stem cell transplant. She has Lebanese heritage and couldn’t find a full match, instead having a – now less common – procedure from umbilical cord cells. She has been in remission since 2012.

Nim Sundaram is undergoing treatment for lymphoblastic leukaemia, There isn’t currently a bone marrow match for him on the registry.Credit: Steven Siewert
For blood cancer patients such as Nim Sundaram, a transplant represents a safety net if other treatments are unsuccessful.
The 28-year-old Sydneysider is in his fourth block of chemotherapy after being diagnosed with lymphoblastic leukaemia just weeks after running the New York Marathon in November.
He has been in remission, so doctors hope he will not need a transplant. He has a partial match with his siblings, but he is yet to find a full one. “It’s purely just based on the luck of who has signed up to the registry,” says Sundaram, who has Sri Lankan heritage.
“All it takes is someone who’s a match with me to have their cheek swabbed, and in five minutes my entire life changes.”

Nikiya Love is one of many Australians with European ancestry who find a bone marrow donor match in Germany.Credit: Steven Siewert
Nikiya Love was 16 weeks pregnant when unusual light-headedness, shortness of breath and stomach cramping led her to the emergency room out of concern for her baby.
She was diagnosed with leukemia and immediately started chemotherapy. She lost her daughter, Lexi, just two weeks later.
Love later had a successful bone marrow transplant, from a donor from Germany, where 10 million are registered. It resulted in a common, but still extraordinary, consequence – her blood type changed, from O negative to A positive – and a remarkable coincidence. Her donor, whom she was allowed to connect with two years after her procedure, shares Lexi’s birthday.
“What do you say to somebody who gives you another chance at life?”
“I don’t really think that there are words big enough.”
How can I donate?
- Enrol with Stem Cell Donors Australia or book a blood donation through Australian Red Cross Lifeblood.
- Choose between providing a sample via a home-delivered cotton cheek swab or blood draw. The sample determines tissue and blood type, as well as the human leukocyte antigen (HLA) markers, proteins present on most of the body’s cells. This data is added to the registry.
- If you’re a potential match for a patient in Australia or worldwide (donors consent to having their match information shared anonymously with transplant teams across the world), you’ll undergo further blood testing and assessments.
- Donors who are selected and cleared by a patient’s medical team undergo one of two donation procedures. The most common is an outpatient procedure where a needle is placed in each arm, one drawing blood, from which a machine separates stem cells, and another returning the remaining blood. Donations where bone marrow is drawn directly from the hip under general anaesthesia are less common, but often requested for paediatric patients.
Most Viewed in National
Loading