It could start when a farmer comes home sick in a small village in the Namakkal district of southern India, where 70 million chickens lay 60 million eggs a day.
Perhaps a colleague who works on one of the region’s 1600 poultry farms also falls ill with the mysterious flu.

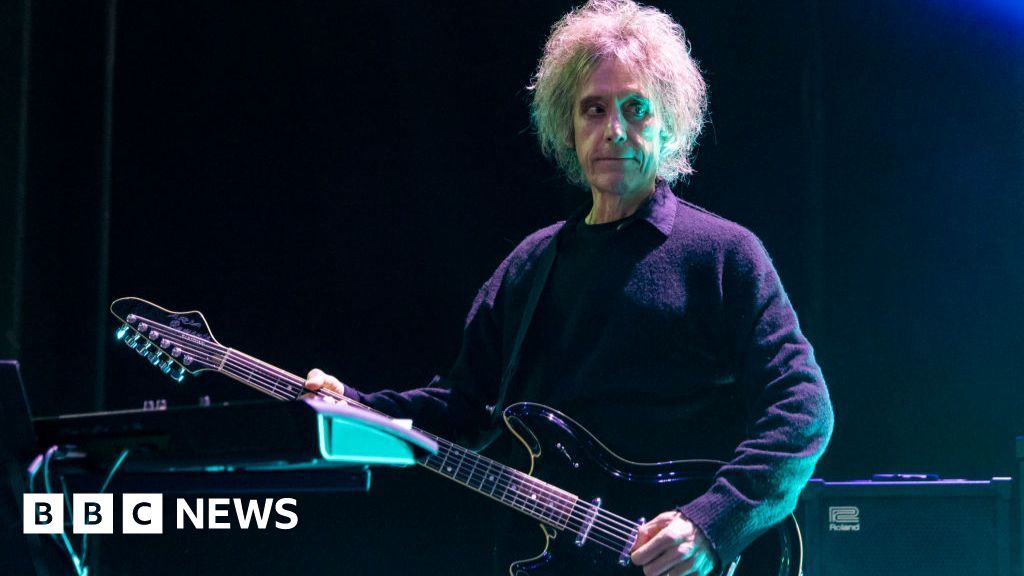
A new study has identified how many cases of bird flu would give way to an outbreak if the virus mutated to spread between humans.Credit: Michael Howard
At this stage, a bird flu pandemic among humans could be contained, if those infected and their close contacts are strictly quarantined.
If more than two fall ill, the risk of wider infection rears its head, according to a new modelling study that simulated what could happen if the virus mutates to spread between people.
Once 10 people have the virus, no means of local containment, bird culling or quarantine will suffice: a widespread outbreak is all but assured.
“It is in the very early stages of an outbreak that control measures make the most difference,” the researchers from Ashoka University in India wrote.

An electron microscope image showing avian influenza virus particles (yellow).Credit: CDC via AP
“Once community transmission takes over, cruder public health measures such as lockdowns, compulsory masking and large-scale vaccination drives are the only options left.”
The researchers used real-world data and repurposed a COVID-19 simulation program to predict how an outbreak of H5N1 bird flu could flare into a pandemic.
It took only 10 active cases to mark the threshold beyond which early containment was as effective as doing nothing, the results of the modelling study in BMC Public Health found, highlighting the slim window of opportunity authorities would have to clamp down on a human-transmissible mutation of the virus.
In the real world, humans remain a dead-end host for the virus: we can catch the disease from animals but we can’t easily pass it on to other people.

H5N1 has hit elephant seals on Heard Island, a sub-Antarctic Australian territory, scientists confirmed in November.Credit: Matt Curnock
There is no evidence the virus has gained the ability to spread from human to human, or spread through the air. These mutations may never arise, said biostatistics expert Professor Adrian Esterman from Adelaide University. The World Health Organisation says the risk to public health from bird flu is low.
But the more bird flu circulates within wild and farmed mammal populations, the more likely unwanted mutations could arise.
The problem H5N1 clade 2.3.4.4b of the virus has remained best adapted to target cells in the guts of birds, but it has repeatedly leapt from waterfowl and poultry to devastate mammals including sea lions, foxes, dolphins and farmed minks.
Infection between cows in the US is a major concern for those worried about a potential sustained leap into humans. Another new study in Nature confirmed newer variants of the virus are better at infecting cow cells and tissues.
“The better adapted they become to infect mammals, the more chances they have to infect and adapt to humans – as we saw with the 2009 swine flu pandemic,” said Professor Pablo Murcia, from the MRC–University of Glasgow Centre for Virus Research and co-author of the research.

Avian flu jumped into cattle for the first time in Texas last year.Credit: AP
A mutation in a single amino acid could be enough to let the virus bind to human cells in the upper respiratory tract rather than bird guts. (One study found the virus circulating in cows can bind only weakly to human cells.)
Other important changes would be needed to sustain human-to-human infection, including airborne transmission.
Symptoms in humans can include high fever, muscle aches and conjunctivitis. There are about 1000 cases of humans becoming injected with bird flu since 2003 with a mortality rate of about 50 per cent, although this is probably overestimated because many asymptomatic cases would have gone unreported, Esterman said.
At least 71 people have caught the virus in the US since the outbreak started last year, and two have died – one in January from H5N1 and another, from a different type called H5N5, in November.
In May 2025, the Trump administration scrapped a $US700 million ($1.05 billion) contract awarded to Moderna to develop and clinically test its bird flu vaccine, designed to fight a potential human pandemic.
But in late December, the Coalition for Epidemic Preparedness Innovations stepped in to fund Moderna’s phase 3 clinical trials of the vaccine with $US54.3 million.
Loading
The trial will take place in the US and Britain to test the safety and efficacy of the RNA vaccine.
“In the event of an H5N1 influenza pandemic, Moderna’s Australian manufacturing facility would work to support the national response by manufacturing an approved H5N1 product, subject to regulatory authorisation and government direction,” the company said in a statement.
Australia remains the only continent spared from an incursion of the problem clade of the virus, which has wiped out millions of birds and other animals.
The virus has, however, hit elephant seals on Heard Island, a sub-Antarctic Australian territory 4000 kilometres from Perth.
The Examine newsletter explains and analyses science with a rigorous focus on the evidence. Sign up to get it each week.
Most Viewed in National
Loading