Madeline Scott knows the reality of rare cancers, as well as the need to multiply efforts to better understand and combat them.
Her daughter Audrey was diagnosed with the rare and aggressive brain cancer medulloblastoma soon after her first birthday in March and, on Anzac Day, she had a 4.5-centimetre tumour removed.

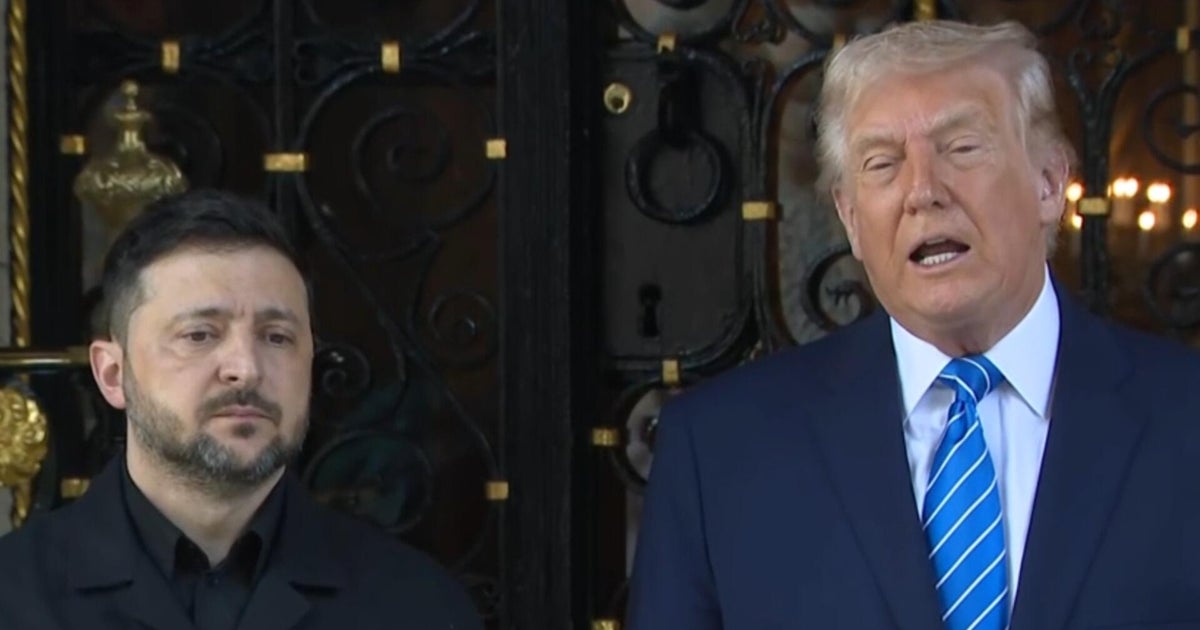
Audrey has a rare form of brain cancer.Credit: Penny Stephens
Since then, the Frankston toddler has spent far too long in the Royal Children’s and Monash Children’s hospitals undergoing imperfect treatments that offer little for the 5 per cent to 15 per cent of cancer patients with a rare form of disease.
“Given the blood-brain barrier, and given Audrey’s age, she’s not able to have radiation therapy,” Scott said. “Chemotherapy-only protocols are quite difficult to treat children like Audrey with, these types of tumours with ... so her tumours are all through the front of her brain and down her spine as well.”
The family is now focused on a project being led by the Children’s Medical Research Institute, which has received a $5 million National Health and Medical Research Council Synergy Grant to improve the treatment of rare and aggressive “ALT cancers”, including bone and soft tissue sarcomas, some pancreatic cancers and many aggressive brain tumours.
“Research is really the only way that we’re ever going to find a cure, and it’s through projects like this that then allow breakthroughs to happen,” Scott said.

Audrey with parents Sam Tunks and Madeline Scott and brother Elliott, 3.Credit: Penny Stephens
Globally, ALT cancers claim up to 1.3 million lives every year including those of 5000 to 7000 Australians, and for parents like Scott anything that can help unlock more secrets about rare disease brings fresh hope.
In the most simple terms, cancer cells kill because they have found a way to override a cell’s normal off-switch and continue to replicate without limit, though how this happens in some rare cancers had long eluded scientists.
The mechanism used by this form of cancers to bypass the off switch is called alternative lengthening of telomeres, or ALT, which was first discovered by Children’s Medical Research Institute-led scientists in the mid-1990s.

Professor Hilda Pickett of the Children’s Medical Research Institute.
With the backing of the NHMRC Synergy Grant, the institute’s Professor Hilda Pickett is leading research to try to turn that discovery into potential treatments through a process that she likens to preventing shoelaces from fraying.
The chromosomes in healthy cells have a sort of cap on their ends called a telomere which keeps them short and prevents them reproducing endlessly, like the aglet, or plastic cap, on the end of a shoelace. But in ALT cancers the aglet has worn off and a mechanism within the cell prevents its end from being effectively sealed, driving its DNA engineroom to endlessly replicate.
“We’re trying to target these mechanisms because, if you disrupt them, then the cells became incredibly unstable and essentially die,” Pickett said.
“It’s a sort of DNA replication engine that we’re looking at, which is specific to these odd cells. We want to try and characterise it structurally and mechanistically to see what it does, and then we can start trying to target different components of this replication engine to try and treat these cancers.
“There’s a couple of proteins that we know that if we target them we get really, really striking outcomes to the cancer cells that use this pathway, and they’re very rapid. And we think it’s a really, really good therapeutic option.”
The multidisciplinary team will also involve researchers from Melbourne’s St Vincent’s Institute, the University of Sydney and the University of Wollongong, and a European-based start-up company that has been created to develop therapeutics specifically targeting ALT cancers.
While they are a long way from knowing if they will one day be clinically ready, Pickett said the researchers already had some preliminary molecules they are examining to see if they can be used to stop the ALT replication engineroom as a promising start for future treatments.
“A lot of these cancers affect young people, and they haven’t really had very improved treatment regimes over decades,” Pickett said.
“The ALT mechanism itself has eluded scientists for a long time, but we’re really making strides at the moment to try and understand the pathway and also to develop treatments which haven’t really been achievable before.
Loading
“We’re looking for new developments – maybe not immediately because things do take a long time, and things always turn out to be quite complicated to take the discoveries through to the actual drugs and the actual clinical testing – but we’re super-hopeful.”
The project is one of 11 funded through the $55 million Synergy Grants scheme this year.
Federal Health Minister Mark Butler said the grants were focused on tackling some of the toughest health challenges.
“This investment will help turn groundbreaking discoveries into real treatments that improve the health and wellbeing of Australians,” Butler said.
While Madeline Scott understands it can be a long and difficult road before research leads to treatment, she also knows the efforts being replicated around the world offer the best hope for patients like Audrey.
“So much can change in 12 months, and that’s the hopeful part. There is so much research and things going on and everyone is putting in towards treatments and research, so I guess that hope is what you hold on to,” Scott said.
Start the day with a summary of the day’s most important and interesting stories, analysis and insights. Sign up for our Morning Edition newsletter.
Most Viewed in National
Loading