When Hamna Aftab was 28 weeks pregnant – anxious and haunted by traumatic birth stories – she met midwife Amar Hamed.
“I just always had a really good feeling about you,” Hamed says to Aftab, whose five-month-old daughter Lulu naps in a carrier on her chest.

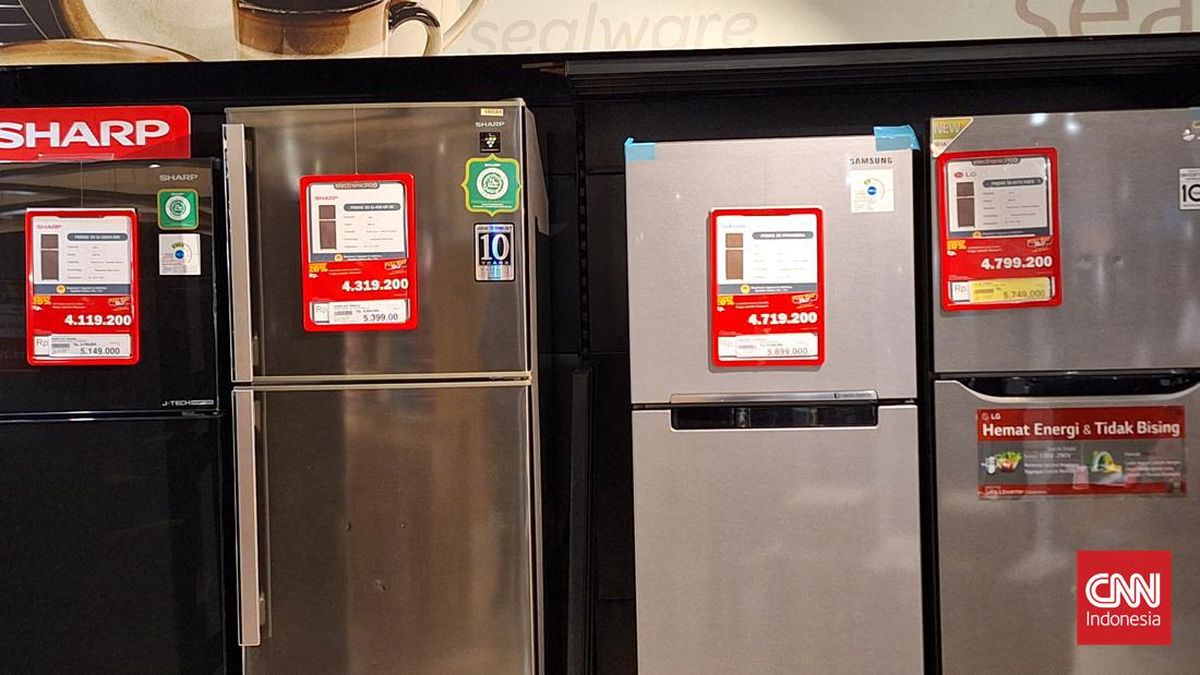
Hamna Aftab, left, trusted midwife Amar Hamed would advocate for her and her baby, Lulu.Credit: Edwina Pickles
There’s an easy warmth between the two women cooing over the baby.
“I remember Hamna’s birth very vividly because I was just like, ‘this is why I’m a midwife’,” Hamed says.
Aftab was among the first women to join Auburn Hospital’s new Midwifery Group Practice (MGP), which offers continuity of care with a primary midwife – through pregnancy, birth and two weeks postpartum – in one of Australia’s most diverse areas.
Loading
The team of four midwives can support 144 women each year, about one in five of all births at the hospital, including refugees, new migrants and women affected by female genital mutilation (FGM), a practice inflicted on girls, usually from infancy to adolescence, where their external genitalia is partially or totally removed or damaged for non-medical reasons.
To date, 138 women have been recruited and 66 babies have been born. Almost half the mothers were born overseas, including 17 per cent from South Asia, 11 per cent from Central Asia and 1 per cent from the Middle East.
Aftab tears up recalling her “beautiful birth” surrounded by her sister, mother, husband Mahmoud and Hamed.
“It was so calming. I did not know that birth could be like that,” she says. “There was a time when I thought, ‘I am going to just die from the pain’, and miraculously [Hamed] pulled me through it.”
Aftab moved to Australia from Pakistan 15 years ago after finishing high school. Her much-wanted pregnancy stirred deeply personal trauma she keeps private but felt safe telling Hamed.
“A lot of my anxiety was because [my baby] is a girl. I don’t want the same things to happen to her,” she says.
“There was a stability with Amar. I could have had a big cry to her because I trusted her with my big emotions.”
“You’ve had a really rough life,” Hamed says to Aftab. “When you meet someone that you can build a relationship with, provide culturally sensitive care, it is the most amazing feeling.”
Both Aftab and Hamed are Muslim, and Hamed’s ability to speak Arabic with Hamna’s introverted husband encouraged him to take part in the birth.
The NSW Birth Trauma inquiry identified midwifery continuity of care as the gold standard, with research showing that having continuity of care with a known midwife yields benefits for mother and baby in the delivery room and the long term. Yet demand for such programs far exceeds availability, which is limited to women who meet low-risk criteria.

Hamna Aftab and her baby, Lulu, with midwife Amar Hamed at Auburn Hospital.Credit: Edwina Pickles
Hamed, who was born at Auburn Hospital and previously worked at Westmead Hospital’s MGP, says helping families navigate cultural and faith-based rituals was part of her role.
“Muslims believe that [the call to prayer called] the adhan should be one of the first things babies hear. It’s a standard practice but non-Muslim practitioners can struggle to find the right time for this,” she says.
Eleven women with FGM have sought antenatal care at Auburn this year. By 2026 the goal is for all eligible women with FGM to be supported under the MGP model.
The program builds on years of work at Auburn to create a maternity model that best supports women with FGM.
Hamed and her colleagues are trained in trauma-informed care and collaborate with an obstetrician to manage severe cases that require surgical reopening of the vaginal entrance, called deinfibulation.
“A lot of these women don’t understand what happened to them … violence without consent. They were really young and it became a huge source of trauma,” Hamed says.
Angela Dawson, a professor of public health at University of Technology Sydney, said it was fantastic that Auburn Hospital is training these midwives to be confident in caring for these women and taking the time to engage with them.
“We need to scale this up,” Dawson said. Her work has shown midwives can be fearful of re-traumatising these women, who express feeling like oddities on display.
Loading
Roughly 53,000 women and girls in Australia have experienced FGM, likely an underestimation. Dawson calculates about 17,000 are in Sydney.
“You’re going to get a lot of presentations across western and south-western Sydney, which probably has the most diverse populations in Australia,” she said.
“There is a risk of poor health outcomes, including tearing and obstructed labour … and they can also experience ongoing chronic pain and psychosexual issues.”
The NSW government allocated $44.8 million in the 2025-26 budget to expand midwifery continuity-of-care models.
Health Minister Ryan Park said: “We want all women in NSW to have access to respectful, evidence-based maternity care, and the establishment of the [MGP] at Auburn Hospital is an important step in achieving this.”
The Morning Edition newsletter is our guide to the day’s most important and interesting stories, analysis and insights. Sign up here.
Most Viewed in National
Loading