Opinion
September 21, 2025 — 5.35pm
September 21, 2025 — 5.35pm
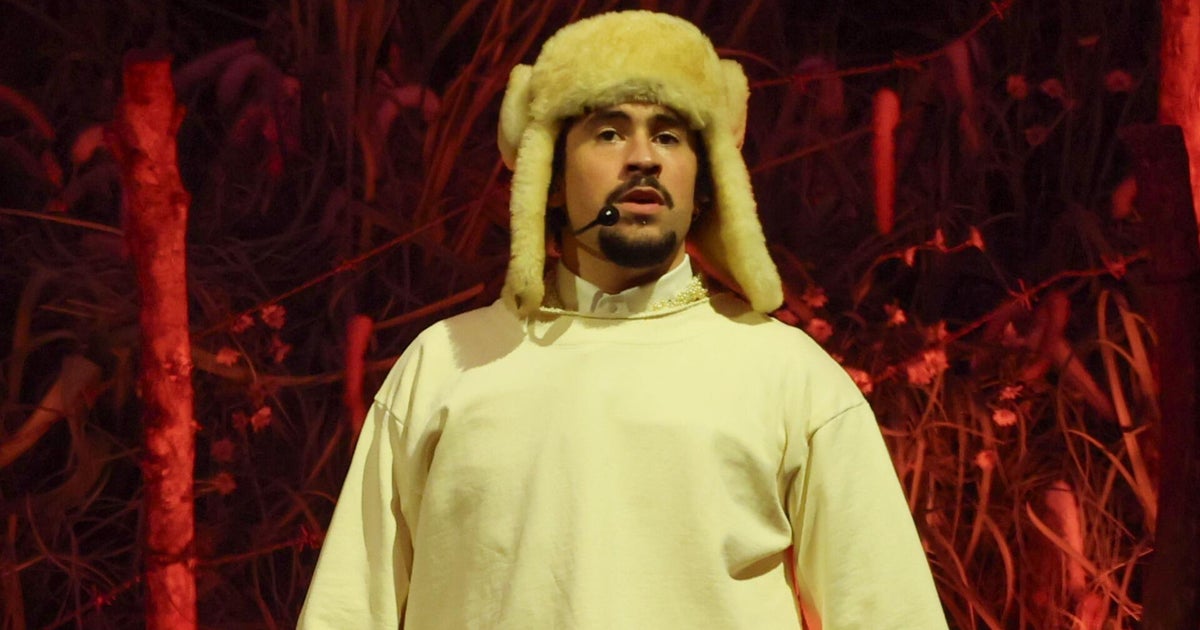
A little over four years ago, I found myself sitting tearily on a hospital trolley, a blue gown pulled tightly across my belly. At the time, I was 16 weeks pregnant and waiting to be wheeled to the operating room.
I’ll get through this, and then it’s done, I remember thinking. I’ll be back to a normal, healthy pregnancy.

Grace was four months pregnant when she had her first emergency surgery, with 15 more to follow in the coming years. Credit: Getty Images
What I didn’t know then is that between that day and now, I’d end up having 16 surgeries. Or that I’d eventually be diagnosed with an aggressive form of Crohn’s Disease, which I’ll be managing forever. Or that I’d see at least 10 specialists in six hospitals, as complications from my illness crept over my body and engulfed my life.
On that day in July 2021, all I knew was that I was on that trolley after I had developed sudden, severe pelvic pain a couple of weeks earlier.
My pelvis and backside felt deeply bruised and tender. I struggled to sit in most positions, and the pain kept me up at night. When I told a doctor this, they quickly diagnosed me with “an overactive pelvic floor” and suggested that I “see a physio, look into relaxation techniques, and work on your stress levels”.
Loading
I left that appointment feeling shrugged off, and as if that diagnosis wasn’t quite right. As it turned out, it wasn’t.
When I saw another doctor for a second opinion, I discovered the real cause of my pain: a large, infected abscess growing in my pelvis that needed emergency surgery.
It turned out that abscess was caused by Crohn’s – a chronic autoimmune condition and a form of Inflammatory Bowel Disease that affects about 180,000 people in Australia. The disease affects men and women in roughly equal numbers, but women tend to wait longer for a diagnosis and are more likely to be misdiagnosed, as I was.
In the four years since I sat on that hospital trolley awaiting my first surgery for that abscess, I’ve encountered more than one doctor who seemed genuinely bamboozled about how to manage my (pregnant, then later lactating) body.
Most of the doctors I came into contact with were male (85 per cent of bowel surgeons in Australia are men). Still, my female physiology puzzled the healthcare professionals, no matter the gender.
I woke up from another surgery later in my pregnancy, distressed to find I’d been repositioned onto my back – a position that increases the risks of stillbirth in later pregnancy. I’d specifically requested not to be placed that way, the surgeon had agreed to this before surgery, but nobody explained why this had been dismissed.
Then there was the way my Crohn’s diagnosis was confirmed, a few months after my son was born. The news was delivered by a stern male surgeon who loomed over my hospital bed, reprimanding me about my choice of gastroenterologist (I’d chosen one he didn’t normally work with; for this, apparently, I needed chiding like an errant child). Throughout his lecture, I grasped groggily at my hospital gown in an attempt to cover my bare breasts; I’d been trying to express milk at the time.
As that white-coated, white-haired doctor towered over me, the message I received was crystal-clear: My agency, privacy and dignity was not his priority.
Loading
There were other lessons awaiting me, too. I learned to time breastfeeding around taking post-operative painkillers. I mastered pumping milk one-handed, while hooked up to IV drug infusions. I learned I had no say in when to stop breastfeeding.
I also learned how hard unwell women have to struggle to be heard. Since I was wheeled into the operating theatre four years ago, I’ve had to advocate relentlessly for myself in a healthcare system that wasn’t made for my body.
Medical science still has gaping, woman-shaped knowledge gaps in its evidence base. Most doctors want to help patients, yet they’re still being taught from textbooks that don’t generally account for sex and gender differences. Recent research from James Cook University found that there is still “no fixed or explicit requirement to include women’s health in Australian medical school curricula”.
As a result, there is a lot that many doctors don’t know about the topics that could have helped me – and other patients like me.
Among those topics: how hormonal shifts, including pregnancy, affect autoimmune disease; how to safely treat pregnant, lactating and newly postpartum patients; how to deal with medical uncertainty, instead of telling women to work on their stress levels.
And above all: Why it’s crucial to listen to women, who have been sidelined by the male-dominated medical system for too long.
Grace Jennings-Edquist is an award-winning journalist, author and host of the podcast Beyond Hysterical.
The Opinion newsletter is a weekly wrap of views that will challenge, champion and inform your own. Sign up here.
Most Viewed in Lifestyle
Loading